A Three-step
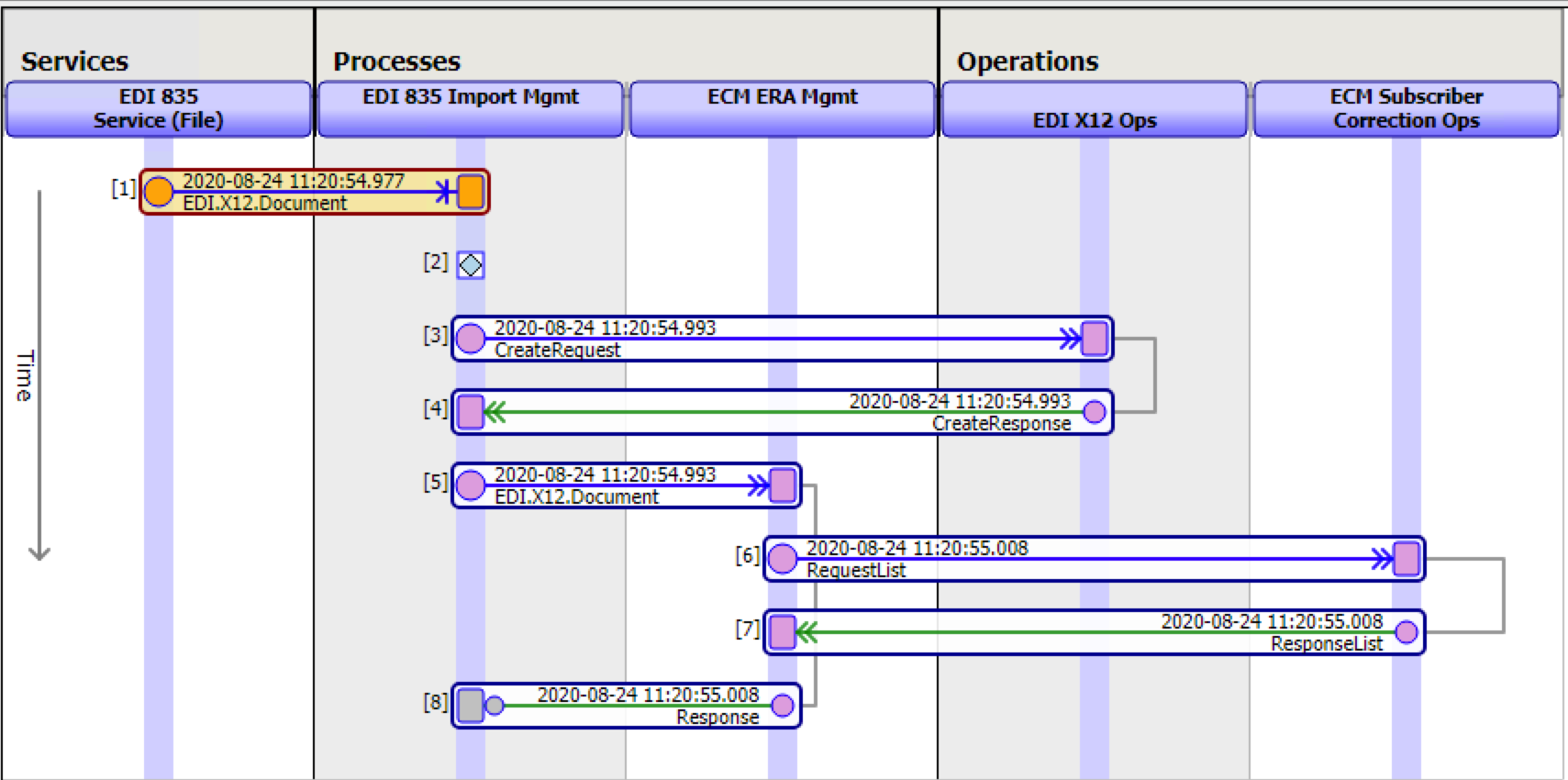
Our goal is to engage with visionary provider organizations on a long-term basis to not only establish a business relationship but to build a community that advances best practices regarding the business of medicine. As with providing care, we believe the best decisions are informed decisions. As such, as a first step, we sign a Business Associate Agreement so that our prospective clients can provide us two types of EDI files – covering a 90-day period.
The first type is Electronic Remittance Advice (ERA), also referred to as EDI X12 835 Transaction Set. The second type consists of electronic claim files. ECM accepts and processes all three types of EDI claim files – 837P, 837I, and 837D for the professional, facility, and dental claims in respective order.
As EDI files are upload to ECM in a mutually agreed upon secured manner, ECM process all files received. Within 10-business days a call is scheduled with management to review the defects identified by ECM and the projections of gains in collections if ECM is to be deployed, completing the first step of ECM Success Methodology.
In reviewing the analysis provided by ECM – based on providers’ actual operating data, management is able to make an informed decision if proceeding with a Proof of Concept (PoC) may be appropriate. If so, an order for a 90-day trial of ECM along with the respective Statement of Work (SoW), which outlines the work to be completed, is executed. The PoC provides revenue operation staff full access to ECM and its capabilities. The PoC is at a fixed fee and covers the ECM 90-day subscription licensing, and professional services as outlined in the SoW. This allows revenue operations staff to incorporate ECM into their daily workflows and existing systems and processes – and management to measure performance and improvements.
With the PoC Agreement in place, provider management simply needs to authorize CHC to be a submitter of Claim Status Inquiry (CSI) Requests (EDI 276 Transaction Set) to Medicare on behalf of the provider organization- the payer activated during the PoC. This generally takes a few minutes to complete and is activated within 24-48 hours.
With CHC authorized with Medicare as a submitter and thus ECM is able to electronically submit claim inquiries, users are trained and a date is set to go live. No migration. No integration. No impact on current systems.
At the start of the PoC, the daily upload of EDI files begin and ECM steps in as a virtual Accounts Receivable team member identifying defects, prioritizing them, and routing them to be fixed. Additionally, it starts following up all Medicare claims at the line item level – regardless of the claim amount. Based on the responses it receives, it identifies problem line items, prioritizes, and routes each problematic claim to be fixed and resubmitted – all well with time limits imposed. Working as a virtual AR member, the chance of missing even a single line item that requires follow-up is zero.
From day one, real-time reporting and analysis are available. The analysis is based on payers’ adjudication data and real-time user productivity. This gives both ECM and management visibility to take corrective actions and continuously and incrementally make improvements. Improvements that lead to lower defect rates and higher yields (collection/net revenue).
As the 90-day PoC comes to an end, management again, based on real data has visibility to make an informed decision if they would like to engage ECM on an annual basis and roll-out it’s capabilities across the enterprise, and for all payers that support electronic claim status inquiries.
Welcome to the dawn of digitalization – driving revenue optimization.